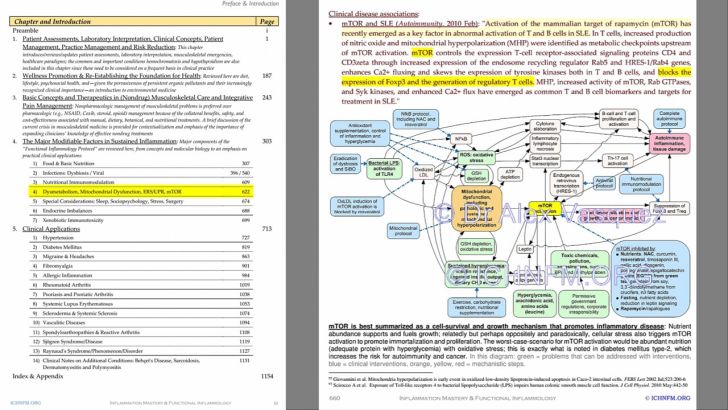
Intracellular Hypercalcinosis: A Functional Nutritional Disorder with Implications Ranging from Myofascial Trigger Points to Affective Disorders, Hypertension, and Cancer
Let’s talk about five pathways by which increased intracellular calcium promotes disease, then let’s talk about THE SOLUTIONS to this common problem
Let’s talk about five pathways by which increased intracellular calcium promotes disease, then let’s talk about THE SOLUTIONS to this common problem
This article was originally published in Naturopathy Digest in 2006 and later reprinted in Inflammation Mastery 4th Edition
Introduction:
Let us explore the possibility that elevated levels of calcium within the cell (intracellular hypercalcinosis) might predispose toward a wide range of clinical problems including migraine, hypertension, myofascial trigger points, inflammation, and cancer. Further, let’s review the data showing that several commonly employed nutritional interventions can be used synergistically to counteract and correct this problem. By the time readers complete this article, they will have 1) an understanding of this problem, 2) a protocol for how to correct this problem, and 3) be able to explain the biochemical rationale for using these nutritional protocols in patients who might otherwise be treated with drugs in general and calcium-channel-blocking drugs in particular.
Although prescription drugs are often used by medical doctors in a “willy-nilly manner” (according to Harvard Medical School Professor Dr. Jerry Avorn[1]), let’s assume for a moment that legitimate reasons exist for the widespread use of drugs that block calcium channels in cell membranes—the “calcium-channel-blocking drugs.” Although it is counterintuitive to promote health by interfering with the body’s natural function, calcium-channel-blocking drugs are routinely used in pharmaceutical medicine for a broad range of problems including hypertension, heart rhythm disturbances, bipolar disorder, and anxiety/panic disorders. Widespread medical use of calcium-channel-blocking drugs appears to validate the supposition that excess intracellular calcium is an important contributor to these and perhaps other problems. Therefore, if intracellular hypercalcinosis is the problem, then any safe and cost-effective treatment that can correct this problem should be met with the same widespread acceptance given to calcium-channel-blocking drugs, which are universally accepted and utilized in the allopathic “conventional medicine” society. At the very least, we can generally state that all phenomena that contribute to calcium deficiency result in an increase in intracellular calcium levels (the “calcium paradox”) due to the effect of parathyroid hormone, which specifically promotes calcium uptake in cells while mobilizing calcium from bone. Additionally, a few other nutritional influences (such as fatty acid imbalances) modulate cellular calcium balance, and these will be discussed in the section on clinical interventions.
The Problem of Excess Intracellular Calcium:
Although the current author is the first to coin the phrase “intracellular hypercalcinosis”, several other authors have pointed to the problem of the “calcium paradox” and the means by which body-wide calcium deficiency can result in intracellular calcium overload, which triggers a cascade of events leading to adverse health effects. Most notably, the work of Takuo Fujita[2],[3] stands out in its clarity and specificity in linking intracellular hypercalcinosis with disorders such as hypertension, arteriosclerosis, diabetes mellitus, neurodegenerative diseases, malignancy, and degenerative joint disease.
Mechanisms by which intracellular hypercalcinosis contributes to disease have been defined, at least partially. However, we must remember that nutritional disorders never occur in isolation, and that the effects of intracellular hypercalcinosis observed clinically are overlaid with manifestations of the primary nutritional/metabolic disorder. Stated differently, contrary to what the pharmaceutical paradigm’s monotherapeutic use of calcium-channel-blocking drugs would imply, intracellular hypercalcinosis never occurs by itself. For example, if intracellular hypercalcinosis is contributed to by vitamin D3 deficiency, then some of the observed clinical complications of that condition are due to and yet independent from the excess intracellular calcium since the primary problem (vitamin D3 deficiency) causes adverse effects and deficiency symptoms that are independent of its effect on intracellular calcium levels. To better understand the specific effects of excess intracellular calcium, a brief review of a few specific biochemical/physiologic mechanisms by which intracellular hypercalcinosis can contribute to disease is warranted. We must start by realizing that calcium is much more than a “bone nutrient” and that it functions as an electrolyte, intracellular messenger, and regulator of cell replication and metabolism.
Let’s talk about five pathways by which increased intracellular calcium promotes disease:
1. Adverse effects on membrane receptors and intracellular transduction: The concentration of extracellular calcium exceeds the concentration of intracellular calcium by a ratio of 10,000 to one. When intracellular calcium levels rise even slightly, receptors and messaging systems in the cell membrane fail to function optimally. Thereby, increased intracellular calcium can predispose to insulin resistance (via interference with insulin receptors) and can promote neurodegeneration by amplifying the intracellular cascade of effects that follows activation of the brain’s NMDA-receptors (excitoneurotoxicity). More specifically, we must note that the recently discovered “calcium-sensing receptor” (CaR, a G protein-coupled plasma membrane receptor) senses minute alterations in serum calcium levels and then ultimately translates these variations into changes in cellular function, notably alterations in cell replication (think cancer) and eicosanoid production (think inflammation).[4],[5] Given that CaR are found in a wide range of cell types, including those found in bone, the kidneys, and immune system, we can see a pathway by which alterations in calcium balance could be implicated in a wide range of diseases. CaR-mediated alterations in cell function are likely to be complicated by disorders of vitamin D3 nutrition and metabolism (that commonly complicate disorders of calcium homeostasis), which affect an even wider range of cell types including those of the breast, prostate, ovary, lung, skin, lymph nodes, colon, pancreas, adrenal medulla, brain (pituitary, cerebellum, and cerebral cortex), aortic endothelium, and immune system, including monocytes, transformed B-cells, and activated T-cells. This is an example of the complexity involved in understanding nutrition in general and the effects of nutritional deficiency (always multifaceted) in particular.
2. Mitochondrial failure and cell death: According to the most recent edition of the classic text Robbins Pathologic Basis of Disease (pages 15-16), increased intracellular calcium is a major cause of cell death. When calcium levels are increased within the cell, one adverse effect is the inhibition of mitochondrial function. Since calcium is pumped out of the cell in an energy-dependent process, and because dysfunctional mitochondria pour calcium into the intracellular space, calcium-induced mitochondrial failure results in an additional increase in intracellular calcium. Further complicating this problem is the fact that the cell membrane becomes increasingly permeable to calcium as calcium levels increase. Elevated intracellular calcium levels activate enzymes such as ATPase, phospholipase, proteases, and endonucleases that promote cell death.
3. Pro-inflammatory effects of intracellular calcium: The recent finding that intracellular calcium activates NF-kappaB[6] has obvious implications given the pivotal role of NF-kappaB in the promotion of systemic inflammation and diseases such as rheumatoid arthritis.[7] Thus, increased intracellular calcium appears to promote inflammation. This may explain in part how vitamin D3 supplementation (which lowers intracellular calcium levels) exerts its clinically impressive anti-inflammatory and immunomodulatory benefits.[8]
4. Enhanced production of lipid peroxides: Fujita notes that lipid peroxides lead to an increase in cell membrane permeability to calcium, which results in increased intracellular calcium; this activates metabolic pathways that increase oxidative stress, thus leading to a vicious cycle stimulated by the production of additional lipid peroxides. Thus, intracellular hypercalcinosis promotes oxidative stress, which becomes self-perpetuating by this and other mechanisms. Of course, we all know by now that increased production of free radicals contributes to the development of many health problems, such as cancer, cardiovascular disease, arthritis, autoimmunity, diabetes, and other forms of rapid biological aging.
5. Myofascial trigger points, chronic muscle spasm, and increased vascular tone (hypertension): The release of calcium from the sarcoplasmic reticulum triggers muscle contraction and plays a role in hypertension (hence the use of calcium-channel-blocking drugs in the treatment of hypertension), chronic muscle spasm (especially when complicated by magnesium deficiency), and the perpetuation of myofascial trigger points.[9] Reducing the levels of cytosolic and sarcoplasmic calcium promotes muscle relaxation.
Nutritional Interventions to Ameliorate Intracellular Hypercalcinosis:
Now that we’ve reviewed the data implicating intracellular hypercalcinosis as a legitimate contributor to a wide range of clinical disorders and diseases, let’s explore some nutritional solutions.
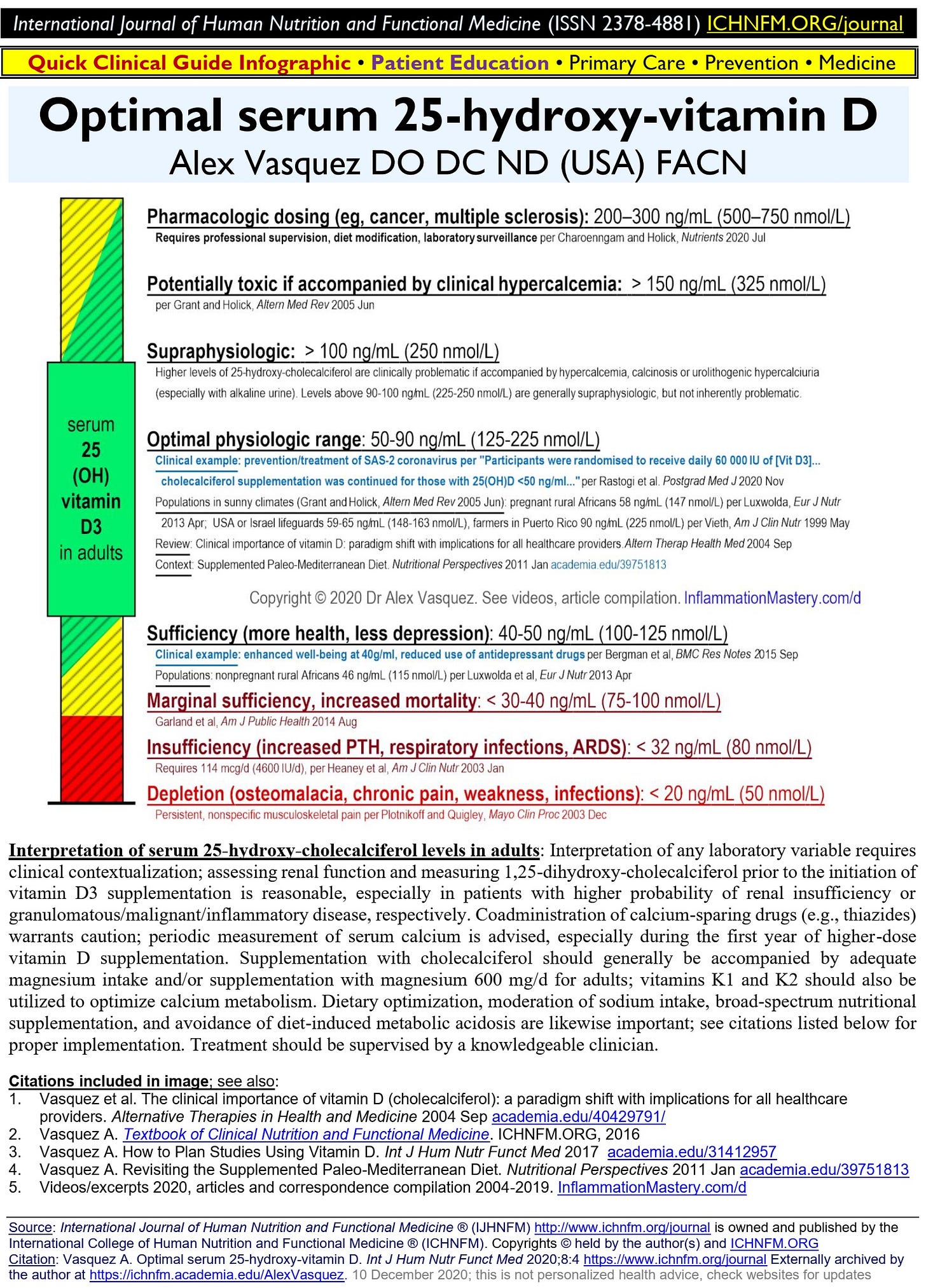
1. Correction of vitamin D deficiency: Vitamin D deficiency causes calcium deficiency which increases parathyroid hormone production resulting in increased intracellular calcium levels. Vitamin D deficiency is common (40-80% of most populations) and can be established via history and more objectively by measurement of serum 25-hydroxyl-vitamin D. Replacement doses are in the range of 1,000 IU per day for infants, 2,000 IU per day for children, and 4,000 IU per day for adults.[10] Vitamin D2 (ergocalciferol) should be avoided, and vitamin D3 (cholecalciferol) should be used, preferably in emulsified form to facilitate absorption, especially in older patients and those with impaired digestion and absorption.[11]
2. Reduction in dietary arachidonic acid intake: Arachidonic acid promotes intracellular calcium uptake, as demonstrated in a recent study using human erythrocytes.[12] Rich sources of arachidonic acid include beef, liver, pork, lamb, and cow’s milk.
Keep reading with a 7-day free trial
Subscribe to INFLAMMATION MASTERY clinical protocols InflammationMastery.com to keep reading this post and get 7 days of free access to the full post archives.