Molecular and Physiologic Mechanisms of Systemic Enzyme Therapy: A Review for Clinicians
Given that the oral administration of pancreatic/proteolytic enzymes for systemic benefits ("systemic enzyme therapy") is one of the most common nutritional/botanical treatments used by integrative clinicians, this article will provide a review of this treatment's clinical benefits and molecular mechanisms, with emphasis on the latter. In this discussion, systemic enzyme therapy or the use of "oral enzymes" will be specified to mean the oral, between-meal administration of supplements containing pancreatin, bromelain, papain, amylase, lipase, trypsin and alpha-chymotrypsin; according to the research literature and clinical experience, polyenzyme preparations are more effective than the use of single enzymes.
Past and Current Use
Systemic enzyme therapy has been used clinically for more than a century, beginning with the early publications of Beard2 and Cutfield,3 who both showed the anti-cancer effects of orally administered enzymes in animals and patients, respectively. Although these and other early reports4-6 showed impressive efficacy and lack of toxicity in the treatment of cancer, they generally were ignored due to enthusiasm surrounding interventional radiation, since "X-rays" had been discovered by Roentgen just a few years earlier and radiation's cancer-causing effects were then unknown.
In this discussion, systemic enzyme therapy or the use of "oral enzymes" will be specified to mean the oral, between-meal administration of supplements containing pancreatin, bromelain, papain, amylase, lipase, trypsin and alpha-chymotrypsin; according to the research literature and clinical experience, polyenzyme preparations are more effective than the use of single enzymes.
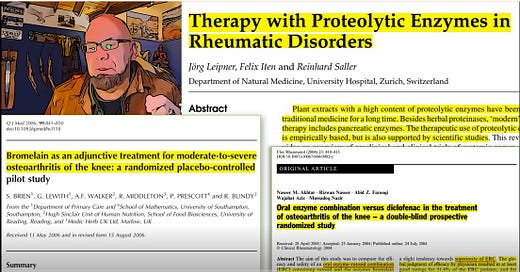
Current clinical uses of pancreatic/proteolytic enzymes are varied, ranging from improved digestion (when taken with meals) to systemic benefits (when taken between meals). Briefly, systemic enzyme therapy commonly is used in the treatment of cellulitis, diabetic ulcers, sinusitis, bronchitis,7-8 injury-related disorders (including contusions, sprains, lacerations, and muscle injuries)9-10 and osteoarthritis (OA).11-12 Use of systemic enzyme therapy in the treatment of cancer is well-supported by experimental and clinical studies.13-18
Paradigm Shift in the Medical Management of Chronic Pain 2024 [#migraine #crps #fibromyalgia #painmanagment #painrelief #paindrugs #chronicpainmanagement #chronicpainawareness]
Updates will be posted here and to https://HealthyThinking.substack.com while this work is being developed and the videos are being edited. Subscribe to get the updates by email!
Physiologic Effects
Physiologic mechanisms of systemic enzyme therapy have been discussed in several of my recent reviews19-21 and will be briefly listed here before advancing to the more detailed molecular mechanisms. Briefly, proteolytic enzymes are well-absorbed from the gastrointestinal tract into the systemic circulation22-23 to exert anti-tumor, anti-inflammatory, anti-edematous and immunostimulatory actions, which are the result of different and synergistic effects, including the following:24-27
dose-dependent stimulation of reactive oxygen species production and anti-cancer cytotoxicity in human neutrophils;
a pro-differentiative effect;
reduction in PG-E2 production;
reduction in substance P production;
modulation of adhesion molecules;
fibrinolytic effects; and
an anti-thrombotic effect mediated at least in part by a reduction in 2-series thromboxanes.
Molecular Mechanisms: New Data
Patients with degenerative and inflammatory arthropathies (e.g., osteoarthritis and rheumatoid arthritis [RA]) have increased synovial concentrations of tissue-destroying proteases such as the matrix metalloproteinases (MMP) and cathepsin B; normally, these proteolytic enzymes are inhibited by endogenous proteinase inhibitors, such as alpha-1-antitrypsin and alpha-2-macroglobulin. Oral administration of pancreatic/proteolytic enzymes such as trypsin and chymotrypsin has been shown to increase serum levels of alpha-1-antitrypsin and alpha-2-macroglobulin, and in this way, oral administration of therapeutic proteases/proteinases stimulates the body's production of endogenous proteinase inhibitors, which then inhibit endogenous joint-destroying proteinases. Stated more simply, systemic enzyme therapy stimulates internal defenses to protect against joint destruction.
Systemic enzyme therapy also modulates cytokine levels and thereby shifts "immune balance" away from the autoreactive cell-mediated Th-1 response and more toward a Th-2 response. Significant reductions in tumor necrosis factor-alpha, interleukin-1b, and autoreactive T-cells have been reported following the administration of oral enzymes in experimental and/or clinical settings. Importantly, systemic enzyme therapy can result in reductions in circulating immune complexes in patients with RA that are directly related to the degree of clinical improvement - the greater the enzyme-induced reduction in immune complexes, the greater the clinical response. This clearly suggests a mechanistic cause-and-effect benefit from systemic enzyme therapy in immune-complex- mediated disease.
However, we also know that RA is a prototype of dysbiosis-induced systemic inflammation28 and thus the recent article by Biziulevicius,29 proposing that the immunostimulatory action of oral enzymes may be derived from direct and indirect intra-intestinal bactericidal and antimicrobial actions, raises an alternate hypothesis that the anti-rheumatic and immune-complex-lowering benefits of systemic enzyme therapy may result not only from intravascular proteolysis of preformed immune complexes, but also primarily from a reduction in de novo immune complex formation due to antimicrobial and thusanti-dysbiotic effects. These effects of systemic enzyme therapy are summarized in Table 1.
Listen to this episode with a 7-day free trial
Subscribe to INFLAMMATION MASTERY clinical protocols InflammationMastery.com to listen to this post and get 7 days of free access to the full post archives.



![Paradigm Shift in the Medical Management of Chronic Pain 2024 [#migraine #crps #fibromyalgia #painmanagment #painrelief #paindrugs #chronicpainmanagement #chronicpainawareness]](https://substackcdn.com/image/fetch/w_1300,h_650,c_fill,f_auto,q_auto:good,fl_progressive:steep,g_auto/https%3A%2F%2Fsubstack-video.s3.amazonaws.com%2Fvideo_upload%2Fpost%2F140912431%2F5b3ff1ea-7d08-4e54-9a48-29e85bb96640%2Ftranscoded-00001.png)